Introduction
Asthma is a chronic inflammatory disorder of the airways, leading to hyperreactivity and recurring episodes of wheezing, chest tightness, and coughing. This condition is caused by airway inflammation, smooth muscle contraction, epithelial shedding, mucus overproduction, bronchial hyperresponsiveness, and mucosal swelling.1
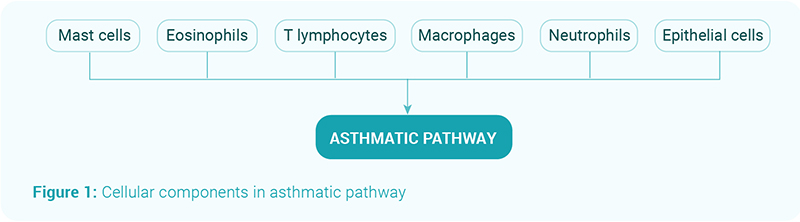
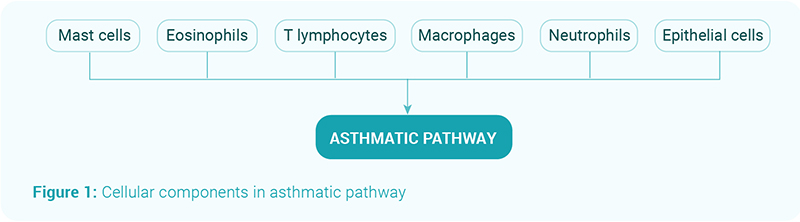
The asthmatic pathway involves various cellular components as shown in figure 1. In susceptible individuals, this inflammation increases bronchial hyperresponsiveness, resulting in episodes of wheezing, breathlessness, chest tightness, and coughing, typically associated with widespread but variable airway obstruction. 2
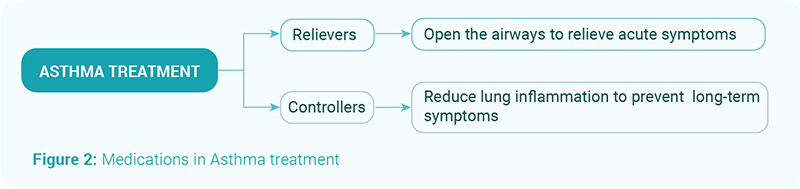
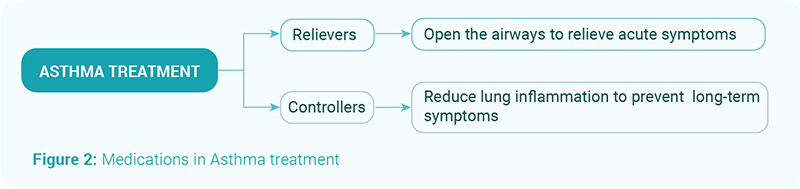
Controller medications include corticosteroids, beta2-agonists, and leukotriene antagonists. The dosage depends on the frequency and severity of asthma symptoms and can be administered via metered-dose inhalers, dry powder inhalers, tablets, or injections. Medications may be combined based on symptom severity.3, 4
The goal of asthma management 4

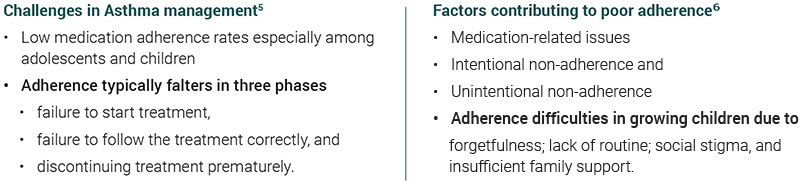
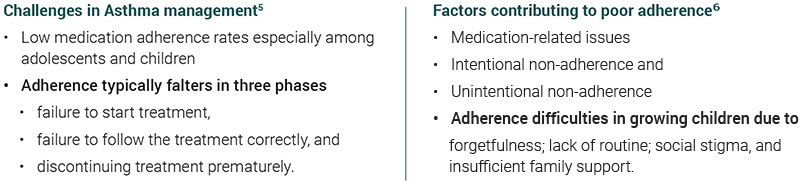
The high medical and social costs of non-compliance have led to renewed interest in addressing this complex issue. 7, 8
Poor adherence to therapy is a major challenge in a treatment strategy that emphasizes early and regular use of controller medications. Patients often hesitate to use inhaled corticosteroid (ICS) controllers regularly, opting instead to manage their asthma symptoms by increasing their use of short-acting beta-agonist (SABA) relievers. This behavior can lead to SABA overuse, increased prescriptions, and a higher risk of asthma exacerbations. 9
Overuse of SABAs 10,11
- Associated with more frequent asthma exacerbations, negatively impacting patient health
- Males, adolescents, and older patients are more prone to SABA overuse compared to females and individuals aged 18-24.
- The use of hypnotics and sedatives, as well as having multiple health conditions, also increases the risk of SABA overuse.
- Excessive use of SABAs lowers patients self-perception of overall and mental health and increases the risk of cognitive and mobility limitations.
- Patient perceptions significantly influence their asthma management and can influence symptom severity.
Studies showing SABA overuse and its consequences
- In one study, SABA overuse was linked to how patients perceived the severity of their symptoms, even though there is often a poor correlation between actual lung function and perceived symptoms.11
- In Sweden, one-third of asthma patients overused SABAs, with 28% not collecting anti-inflammatory medications. Despite the availability of effective controller treatments, SABA overuse persists.10
- A study by Stanford et al. shows that using two or more SABA canisters within six months doubles the risk of an asthma exacerbation. Each additional SABA canister increases the risk by 14-18%.12
Combination Therapy:
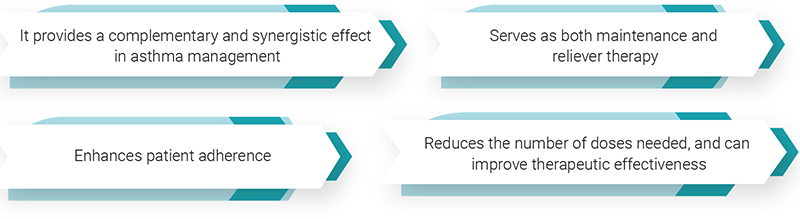
- Several studies have demonstrated that combination therapy in a single inhaler provides complementary and synergistic effects in asthma management.
- Recent research indicates that this combination therapy can be used both as maintenance and reliever therapy, with the same efficacy as short-acting beta-agonists (SABAs).13
Advantages of combination therapy 14,15
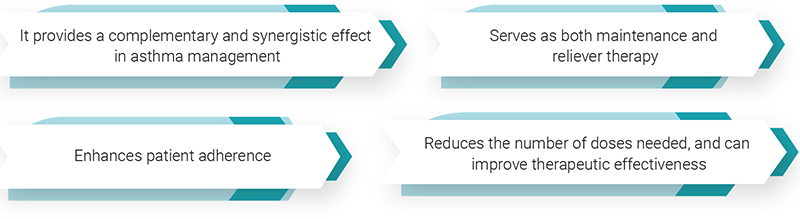
- Combination therapy in a single inhaler device offers several advantages.
- Inhaled corticosteroids (ICS) are the most effective asthma controllers, suppressing inflammation and managing symptoms. A fixed-dose combination in a single inhaler is recommended for patients requiring multiple medications.
Evidences:
- A study by Papi et al. (2007) involving 455 patients with mild asthma showed that using a single inhaler containing beclomethasone (250 µg) and albuterol (100 µg) as needed was as effective as regular use of beclomethasone (250 µg twice daily). This approach was also associated with a lower cumulative dose of the inhaled corticosteroid over six months.16
- Another study by Papi et al. (2022) found that the risk of severe asthma exacerbations was significantly lower with the as-needed use of a fixed-dose combination of 180 µg of albuterol and 160 µg of budesonide compared to as-needed use of albuterol alone. This study included patients with uncontrolled moderate-to-severe asthma who were on various inhaled glucocorticoid-containing maintenance therapies.17
- The BEST study in adults and the TREXA study in children and adolescents further support these findings. The BEST study used a single inhaler combination of beclomethasone and albuterol, while the TREXA study used separate beclomethasone and albuterol inhalers. Both studies demonstrated fewer exacerbations with the as-needed ICS/SABA strategy compared to SABA-only therapy. Additionally, the groups treated with as-needed ICS/SABA used less cumulative ICS and experienced similar or fewer exacerbations compared to those on maintenance ICS therapy for mild asthma.15,18
These studies collectively highlight the effectiveness of combination therapy in a single inhaler, showing that it can serve both as maintenance and reliever therapy, enhance patient adherence, reduce dosage regimens, and improve therapeutic outcomes in asthma management.
Conclusion:
- The use of combination ICS/SABA including of levosalbutamol and beclomethasone therapy in treating asthma offers significant advantages, including enhanced patient adherence, reduced treatment complexity, and improved clinical outcomes.
- Studies demonstrate that this approach effectively controls asthma symptoms, reduces the risk of exacerbations, and lowers the overall use of inhaled corticosteroids.
- Combination therapy, a single device that combines maintenance and reliever medications, simplifies treatment regimens and supports personalized asthma management, making it an ideal strategy for primary care physicians and patients.
- Combination inhaler devices facilitate an individualized approach to asthma management and reduce treatment complexity.
- This makes them ideal for adoption by primary care physicians, enabling patients to effectively achieve control over their condition.
Reference:
- Padem N, Saltoun C. Classification of asthma. Allergy Asthma Proc. 2019;40 (6):385-388. doi:10.2500/aap.2019.40.4253
- National Institutes of Health; National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Expert panel report 3: Guidelines for the diagnosis and management of asthma. Aug 2007
- org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Asthma: Learn More – Medication for people with asthma. [Updated 2022 Jul 15]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279519/
- POCKET GUIDE FOR ASTHMA MANAGEMENT AND PREVENTION: GINA; 2023 [cited 2024 1-Apr-24]. Available from: GINA Pocket Guide 2023 (ginasthma.org)…
- Cochrane M, Horne R, Chanez P. Compliance in asthma. Respiratory medicine. 1999;VOLUME 93, ISSUE 11, P763-769(16-May-24).
- Vrijens B, Dima AL, Van Ganse E, van Boven JF, Eakin MN, Foster JM, et al. What We Mean When We Talk About Adherence in Respiratory Medicine. The journal of allergy and clinical immunology In practice. 2016;4(5):802-12.
- Kaplan A, Price D. Treatment Adherence in Adolescents with Asthma. Journal of asthma and allergy. 2020;13:39-49.v
- George M, Bender B. New insights to improve treatment adherence in asthma and COPD. Patient Prefer Adherence. 2019;13:1325-34.
- Papi A, Blasi F, Canonica GW, Morandi L, Richeldi L, Rossi A. Treatment strategies for asthma: reshaping the concept of asthma management. Allergy, asthma, and clinical immunology : official journal of the Canadian Society of Allergy and Clinical Immunology. 2020;16:75.
- Nwaru BI, Ekström M, Hasvold P, Wiklund F, Telg G, Janson C. Overuse of short-acting β(2)-agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. 2020;55(4).
- Canonica GW, Paggiaro P, Blasi F, Musarra A, Richeldi L, Rossi A, et al. Manifesto on the overuse of SABA in the management of asthma: new approaches and new strategies. Ther Adv Respir Dis. 2021;15:17534666211042534.
- Stanford RH, Shah MB, DSouza AO, Dhamane AD, Schatz M. Short-acting β-agonist use and its ability to predict future asthma-related outcomes. Annals of allergy, asthma & immunology : official publication of the American College of Allergy, Asthma, & Immunology. 2012;109(6):403-7.
- Saleh JA. Combination therapy in asthma: a review. Nigerian journal of medicine : journal of the National Association of Resident Doctors of Nigeria. 2008;17(3):238-43.
- Brunaugh AD, Sharma S, Smyth H. Inhaled fixed-dose combination powders for the treatment of respiratory infections. 2021;18(8):1101-15.
- Asthma, Management and Treatment: CDC; 2023 [cited 2024 4-Apr-24]. Available from: https://cdc.gov/asthma/management.html.
- Papi A, Canonica GW, Maestrelli P, Paggiaro P, Olivieri D, Pozzi E, et al. Rescue use of beclomethasone and albuterol in a single inhaler for mild asthma. The New England journal of medicine. 2007;356(20):2040-52.
- Papi A, Chipps BE, Beasley R, Panettieri RA, Israel E, Cooper M, et al. Albuterol–Budesonide Fixed-Dose Combination Rescue Inhaler for Asthma. New England Journal of Medicine. 2022;386(22):2071-83.
- Martinez FD, Chinchilli VM, Morgan WJ, Boehmer SJ, Lemanske RF, Jr., Mauger DT, et al. Use of beclomethasone dipropionate as rescue treatment for children with mild persistent asthma (TREXA): a randomised, double-blind, placebo-controlled trial. Lancet (London, England). 2011;377(9766):650-7.